If you or someone you know has been diagnosed with esophageal varices, it’s important to understand what they are and how to manage them. Esophageal varices are enlarged veins in the esophagus that can lead to dangerous bleeding if left untreated. That’s why surveillance guidelines have been established to help detect and monitor esophageal varices before they become a serious problem.
In this blog post, we’ll dive into what you need to know about esophageal varices surveillance guidelines, including when to start surveillance, how often to have screenings, and what tests to expect. Knowing this information can help you take a proactive approach to managing your esophageal varices and prevent serious complications.
Understanding Esophageal Varices
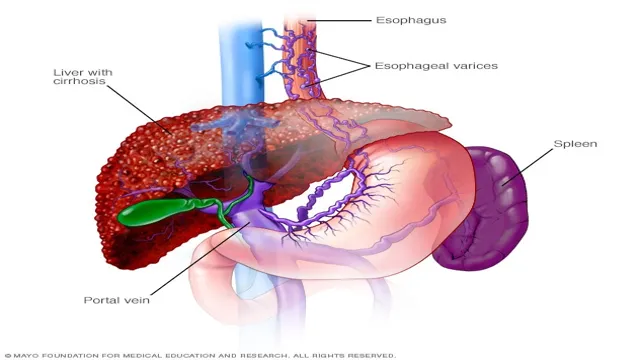
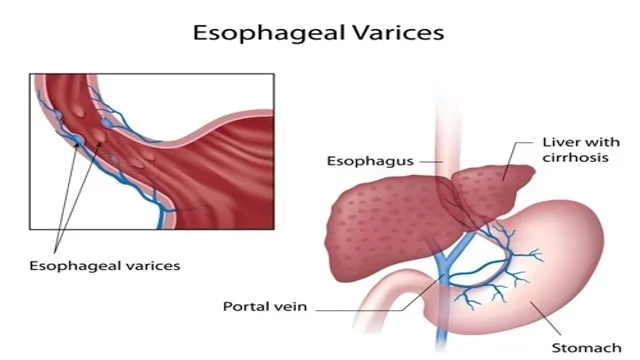
Esophageal varices are enlarged and swollen veins in the lower part of the esophagus, commonly seen in individuals with liver disease. These varices can be life-threatening if they rupture and bleed, which is why it’s crucial to accurately monitor and manage them through regular surveillance. The American Association for the Study of Liver Diseases (AASLD) has issued guidelines for esophageal varices surveillance, which advise endoscopic screening for patients with cirrhosis or other high-risk factors.
These guidelines also outline the frequency and modality of surveillance for different patient populations. Esophageal varices surveillance guidelines are important in managing the condition effectively and preventing potentially fatal complications. If you or a loved one has been diagnosed with esophageal varices, it’s essential to discuss the recommended surveillance plan with your healthcare provider and ensure proper follow-up.
Symptoms of Esophageal Varices
If you have been diagnosed with liver disease, cirrhosis, or have damaged liver tissue, you may be at risk for developing esophageal varices. Esophageal varices are swollen, enlarged veins that develop in the esophagus. These veins are fragile and can burst, causing life-threatening bleeding.
Symptoms of esophageal varices can include vomiting blood, passing black and tarry stools, severe abdominal pain, and difficulty swallowing. It is important to seek medical attention immediately if you experience any of these symptoms. Your doctor may recommend endoscopy to diagnose and treat esophageal varices to prevent further complications.
Maintaining a healthy lifestyle, managing underlying liver disease, and avoiding alcohol and drugs can help reduce your risk of developing esophageal varices.
Prevalence Rates of Esophageal Varices
Esophageal Varices Esophageal varices refer to swollen and enlarged veins that develop in the lining of the esophagus, the tube that connects the throat to the stomach. These veins are a result of increased pressure in the blood vessels that carry blood from the liver to the heart. Esophageal varices are most commonly caused by liver diseases such as cirrhosis, hepatitis, and alcohol-related liver disease.
The prevalence of esophageal varices varies depending on the underlying condition and age of the patient. Studies have shown that in patients with cirrhosis, the rate of esophageal varices ranges from 50-60%, while in patients with hepatitis C, the rate is approximately 30%. The prevalence is higher in older patients and those with a longer duration of liver disease.
Early detection and treatment of esophageal varices are vital as they can rupture and cause severe bleeding, which can be life-threatening. Regular screening and monitoring are necessary for patients with liver disease to identify and manage esophageal varices promptly.
Surveillance Guidelines for Esophageal Varices
If you have been diagnosed with esophageal varices, it is essential to undergo regular surveillance to detect any changes and prevent potential complications. The American Association for the Study of Liver Diseases recommends that patients with medium and large esophageal varices should have an initial endoscopy to confirm the diagnosis and assess the severity of the varices. Afterward, follow-up endoscopies are necessary every one to two years to monitor the progression of the varices and identify any signs of bleeding.
In addition to endoscopy, your healthcare provider may recommend imaging tests such as ultrasound or CT scan to evaluate the liver’s function and assess for other potential complications. By adhering to a surveillance program, you can reduce the risk of variceal bleeding and improve your overall health outcomes. Stay proactive and work closely with your healthcare team to ensure that you receive the appropriate care and monitoring specific to your needs.
Remember, early detection is critical in preventing severe complications that may arise from esophageal varices.
When to Start Surveillance
Esophageal Varices Surveillance Guidelines When it comes to surveillance for esophageal varices, there are a few guidelines that doctors follow to ensure patients receive the best care possible. For patients with cirrhosis, it is recommended to begin surveillance for esophageal varices once they reach the compensated stage, as this is when the risk of developing varices is highest. For patients who have already been diagnosed with varices, surveillance should be performed every 6-12 months to assess the size and risk of bleeding.
If the varices are small and without high-risk features, the surveillance interval can be extended to 1-2 years. On the other hand, if the patient has had a previous bleed or has large or high-risk varices, they may require more frequent surveillance or even prophylactic treatment. It is important for doctors to be vigilant with surveillance for esophageal varices to detect any changes early and prevent serious complications.
Frequency of Surveillance
When it comes to esophageal varices, monitoring and surveillance are crucial. The frequency of surveillance depends on the severity of the varices. For those with small varices, surveillance every 2-3 years is appropriate.
For individuals with medium to large varices, surveillance should be conducted every 6-12 months. It is important to note that these guidelines are not one-size-fits-all, and individual circumstances should be taken into account. For example, if a patient experiences symptoms such as bleeding, more frequent surveillance may be necessary.
Additionally, those with a history of bleeding varices or other liver-related conditions may require more frequent monitoring. Regular surveillance is essential for detecting and treating any variceal bleeding early, which can significantly improve the patient’s outcomes. Therefore, it is essential to work with your healthcare provider to develop a surveillance plan that meets your unique needs.
Remember, early detection is the key to managing esophageal varices effectively.
Surveillance Methods
If you have been diagnosed with esophageal varices, it is important to undergo regular surveillance in order to detect any changes or complications. There are several methods that may be used to conduct surveillance, including endoscopy and ultrasound imaging. Your doctor will determine the most appropriate surveillance method based on your individual needs and medical history.
Generally, surveillance will be conducted every six months to one year, depending on the severity of your condition. During surveillance, your doctor will look for signs of bleeding or enlargement of the varices. If any complications are detected, your doctor may recommend additional testing or treatment options.
It is important to stay up-to-date with your surveillance appointments in order to catch any issues early and ensure the best possible outcome. Overall, following surveillance guidelines for esophageal varices is essential in managing and treating this condition.
Preventing Esophageal Varices Complications
Esophageal varices surveillance guidelines play a vital role in preventing complications resulting from this condition. Esophageal varices can be dangerous and even life-threatening if left untreated, causing bleeding and other complications. However, with proper monitoring and surveillance, medical professionals can detect early signs of varices and take appropriate actions to prevent complications.
The surveillance guidelines vary depending on the patient’s medical history and risk factors for esophageal varices, but usually involve regular endoscopies to examine the esophagus and monitor any changes. Treatment may involve medication to reduce the risk of bleeding or procedures to address the varices directly. By staying up-to-date with esophageal varices surveillance guidelines and working closely with a medical professional, patients can greatly reduce their risk of complications and maintain better overall health.
Lifestyle Changes to Prevent Complications
Esophageal varices can be a serious health concern, but there are steps you can take to prevent complications from developing. Making lifestyle changes is a crucial part of preventing esophageal varices complications. One of the most important things you can do is stop drinking alcohol.
Alcohol consumption is one of the leading causes of esophageal varices, so cutting back or quitting altogether can greatly reduce your risk. It’s also essential to maintain a healthy weight, as obesity can increase your chances of developing this condition. Additionally, managing your blood pressure can help prevent complications.
High blood pressure can damage blood vessels and make esophageal varices more likely to form. By making these lifestyle changes and working with your healthcare provider, you can reduce your risk of complications and maintain your overall health.
Medications and Procedures for Preventing Complications
Esophageal varices are a serious condition that can lead to life-threatening complications if left untreated. Thankfully, there are medications and procedures available that can help prevent these complications from occurring. One common medication used to prevent complications is a beta-blocker, which helps to lower blood pressure in the portal vein and reduce the risk of bleeding.
Additionally, endoscopic treatments such as banding or sclerotherapy can be performed to directly treat the varices and prevent them from rupturing. It is important for patients with esophageal varices to work closely with their doctors to develop a comprehensive treatment plan that includes regular monitoring and preventative measures to ensure the best outcomes. By taking proactive steps to manage their condition, patients can significantly reduce the risk of complications and maintain their overall health and well-being.
Conclusion: Stay on Top of Surveillance and Prevention
In conclusion, following proper surveillance guidelines for esophageal varices is like hitting the bullseye in darts – it may take some patience and precision, but it ultimately reduces the risk of a potentially fatal outcome. So, let’s aim high and stay vigilant in monitoring these pesky varices to ensure the best possible outcome for our patients. Cheers to healthy livers and sharp shooting doctors!”
FAQs
What are the esophageal varices surveillance guidelines?
Esophageal varices surveillance guidelines are recommendations for monitoring and management of patients with liver cirrhosis or other risk factors for developing esophageal varices, such as portal hypertension.
How often should patients with esophageal varices be monitored?
According to the current guidelines, patients with medium to large esophageal varices should undergo endoscopic surveillance every 1 to 2 years, while those with small varices should be monitored every 3 to 5 years.
What are the risk factors for developing esophageal varices?
The main risk factor for developing esophageal varices is liver cirrhosis, but other factors such as portal hypertension, advanced age, male gender, and alcohol abuse may also increase the risk.
What are the treatment options for esophageal varices?
Treatment options for esophageal varices include endoscopic band ligation, sclerotherapy, or transjugular intrahepatic portosystemic shunt (TIPS) procedures. Additionally, medications such as beta-blockers or nitrates may be used to reduce portal hypertension and prevent variceal bleeding.